Anorectal Surgeries: Specialized Procedures for Anal and Rectal Conditions
What are Anorectal Disorders?
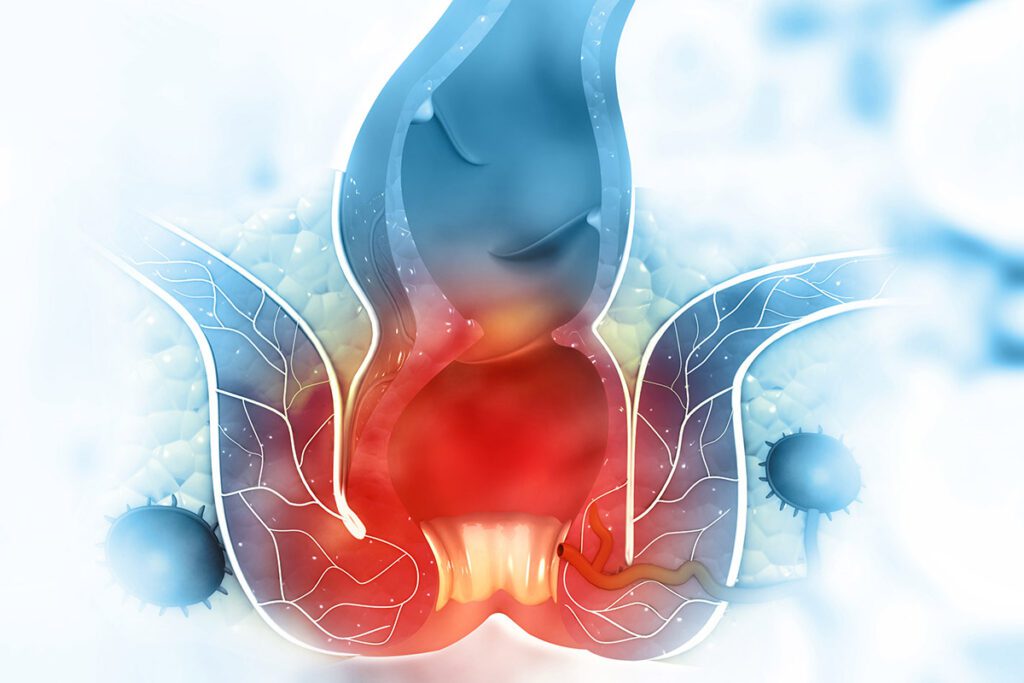
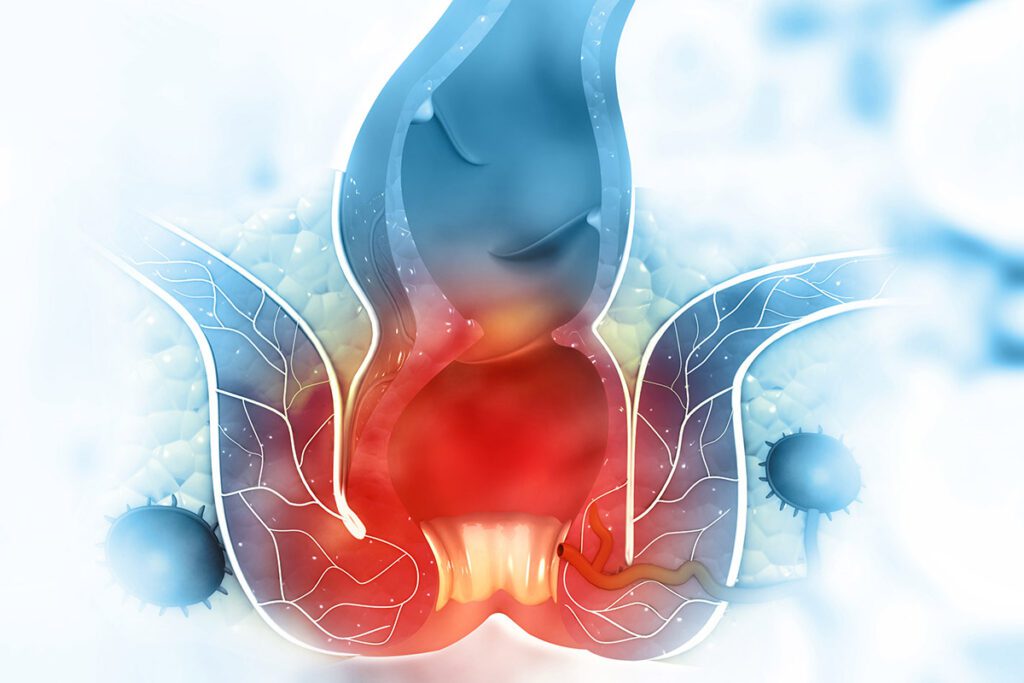
The anus is a complex structure comprised of glands, muscle rings in the anal canal, and an involuntary anal sphincter. Working in harmony, these components control bowel movements. Anorectal disorders encompass various conditions affecting these crucial areas.
Anorectal disorders constitute a range of ailments, such as tears in the anus and rectum, anal fissures, fistulas, hemorrhoids, and even cancer. While most conditions are benign, they necessitate medical attention to prevent potential complications. Unfortunately, individuals often refrain from seeking medical help for anorectal issues, leading to the possible worsening of these conditions.
Identifying anorectal disorders can be crucial. Symptoms often manifest as:
- pain
- itching
- anal bleeding
- swelling
- incontinence
- burning sensation
- presence of blood in the stool
Early detection and proper management are pivotal in addressing anorectal disorders effectively, ensuring timely treatment and relief from discomfort.
Diagnosing Anorectal Conditions
Medical professionals utilize various tools to accurately diagnose anorectal conditions, ensuring a precise understanding of the patient’s health concerns:
- Biopsy: This involves the extraction of a small tissue sample for examination, commonly employed to assess polyps and tumors, determining their nature, whether benign or cancerous.
- Anoscopy: A diagnostic technique employing a small, tube-like instrument equipped with a light inserted into the anus. This allows visualization of the final few inches of the rectum and anal canal.
- Colonoscopy: This procedure involves examining the entire large intestine under moderate sedation. It requires thorough bowel preparation and aids in detecting rectal and colon cancers or abnormalities.
- Flexible sigmoidoscopy: Similar to a colonoscopy but focusing solely on the rectum and sigmoid colon rather than the entire large intestine leading to the rectum.
- Ultrasound or MRI: Non-invasive imaging tests revealing the structure and functionality of the anal canal, sphincter muscles, and rectum.
By employing these diagnostic tools, healthcare professionals can accurately assess anorectal conditions, facilitating appropriate treatment measures tailored to each patient’s needs.
Understanding Anorectal Surgeries
Anorectal surgeries are specialized surgical procedures aimed at repairing or reconstructing the anus. Situated at the terminal end of the large intestine, the anus spans approximately 3-4 centimeters. Encircling it are circular muscles called sphincters, crucial for expelling waste from the body.
These surgical interventions focus on rectifying issues within and around the anus. Some conditions may be congenital, while others result from injury or disease.
At our facility, expert surgeons conduct anorectal surgeries, ensuring precise explanations, specialized care, and tailored surgical procedures to address diverse anorectal conditions effectively.
Types of Anorectal Conditions
At Proliance Surgeons Surgical Specialists of Edmonds, we’ve successfully treated numerous patients dealing with a spectrum of anorectal disorders. Our approach prioritizes understanding your specific concerns, ensuring a comfortable and personalized visit. Common anorectal conditions include:
- Anal Fissure: Often arising from constipation or straining during bowel movements, these small tears in the anal canal can also result from chronic diarrhea. Symptoms include severe sharp pain during bowel movements and bright red blood.
- Anal Fistula and Abscess: An abscess, an infected tissue pocket around the anus, can lead to a fistula—an abnormal connection between the anal canal and the skin. Symptoms encompass pain, fever, redness, and bloody discharge or stool, often necessitating surgical intervention.
- Pilonidal Disease: Occurs when broken hair penetrates small breaks in the skin, leading to inflammation and infection. Symptoms involve pain, redness, drainage, or abscesses in the anal area.
- Hemorrhoids: These are blood vessels in the anal lining that, when inflamed, cause noticeable discomfort, such as bleeding, itching, and pain during bowel movements.
- Pruritis Ani: Commonly referred to as “itchy anus,” serves as a symptom associated with various anorectal conditions such as bacterial or fungal infections, cancer, or chronic skin ailments. This distressing symptom often manifests as severe itching, potentially escalating into pain and stinging sensations.
- Anal Condyloma: Also known as anal warts, is observed in a small percentage of individuals exposed to the human papillomavirus (HPV). While some cases may be asymptomatic, others can cause discomfort, such as itchiness, pain, and bleeding, posing challenges in maintaining proper hygiene.
- Anal Stenosis: a condition where the anal canal narrows, often attributed to the formation of scar tissue that impedes the stretching of anal walls necessary for the passage of feces. This condition may arise as a side effect following anorectal surgery or as a consequence of a chronic, long-term disease.
Recognizing the specific nature of each anorectal condition is vital in providing tailored treatment approaches for our patients.
Types of Anorectal Surgeries
Transanal Endoscopic Microsurgery (TEM)
Transanal endoscopic microsurgery (TEM) is a minimally invasive approach used for the surgical removal of rectal polyps and tumors. Unlike traditional abdominal incisions, this technique involves the insertion of microsurgical tools through the anus. TEM offers enhanced precision, quicker recovery times, reduced scarring, and minimized bleeding and complication risks.
Anal Sphincter Reconstructive Surgery
Anal sphincter reconstructive surgery, or sphincterotomy, addresses anal sphincter tears resulting from childbirth, cancer, incontinence, or trauma. This surgical intervention focuses on rebuilding torn or weakened sphincter muscles and the anus, aiming to alleviate pain and discomfort. Another type of sphincterotomy is anoplasty. Anoplasty involves reconstructing the anus to optimize excrement expulsion, specifically addressing anal stenosis and anorectal malformations.
Anal Fistula Removal
For smaller fistulas, outpatient procedures suffice. Larger fistulas necessitate advanced techniques such as:
- Fistulotomy: Removal of the entire fistula and surrounding tissue.
- Seton Drain: A surgical thread looped through the fistula for drainage or to block the tract, aiding the healing of the surrounding tissue.
- Endorectal Advancement Flap: This procedure is done by excising infected tissue at the inside opening and closing it with healthy rectal tissue while it drains through the outside opening.
- LIFT or Ligation of Intersphincteric Fistula Tract: It is the closure of the fistula between sphincter muscles (commonly by stitches) before the surgeon removes the fistula tract or infected tissue inside.
Hemorrhoidectomy
Severe cases of hemorrhoids may require surgical removal of the hemorrhoid and surrounding tissues, while nonsurgical procedures suffice for milder cases.
Patient-Centered Approach to Anorectal Health: Preparing for Surgery
Before the procedure, the patient must remove artificial objects from their person, such as contacts or dentures. The patient will be in sustained sedation throughout the procedure through an intravenous (IV) line.
Integral components of the surgical process encompass:
- Implementation of a pre-surgery laxative and fasting after midnight to prepare the bowels for the procedure.
- Anorectal procedures may extend over several hours.
- The recovery duration varies, contingent upon the surgery type and individual, with most patients resuming regular activities within one to three months post-operation.
- Implementation of personalized pain management protocols.
- Postoperative care integrates rehabilitation strategies and comprehensive homecare instructions, forming an integral part of the patient-centered approach. Follow-up checkups are imperative to confirm steady recovery and minimal complications.
Our Experienced Anorectal Surgeons
Meet our expert surgeons and anorectal health specialists at Proliance Surgeons of Edmonds.
Carol Cornejo, MD, FACS
- Breast Surgery
- Abdominal Surgery
- Laparoscopic Surgery
- Hernia Surgery
- Thoracic Surgery
Justin Olsen, MD, FACS
- Abdominal Surgery
- Anorectal Disorders
- Hernia Surgery
- Laparoscopic Surgery
- Robotic Surgery
Reach Out to Us for Anorectal Surgery Consultation
Seek consultation at Proliance Surgical Specialists of Edmonds for expert care. Our anorectal specialists are here to give you a prompt diagnosis and efficient treatment. Dedicated to your comfort and well-being, we prioritize your care. Streamlining the consultation process, we address all surgical inquiries and support you through your recovery journey. Reach out to us today to embark on your path to improved anorectal health.











